1
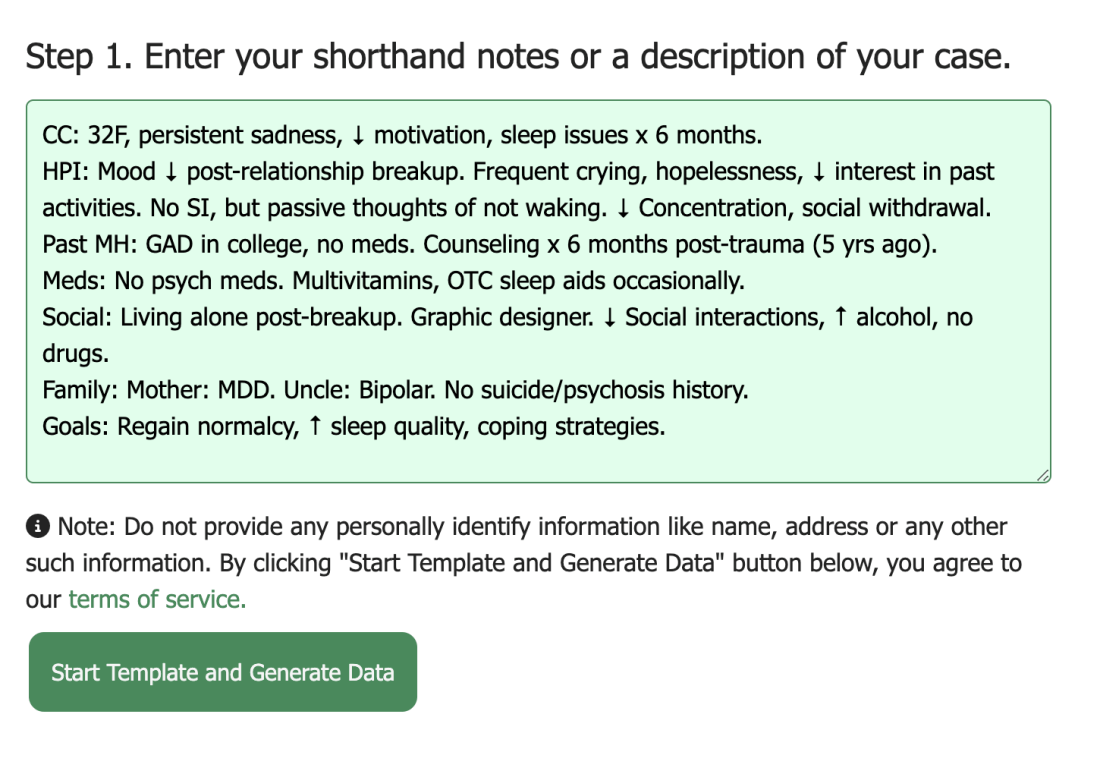
Enter your shorthand notes or a description
For example,
CC: 32F, persistent sadness, ↓ motivation, sleep issues x 6 months.
HPI: Mood ↓ post-relationship breakup. Frequent crying, hopelessness, ↓ interest in past activities. No SI, but passive thoughts of not waking. ↓ Concentration, social withdrawal.
Past MH: GAD in college, no meds. Counseling x 6 months post-trauma (5 yrs ago).
Meds: No psych meds. Multivitamins, OTC sleep aids occasionally.
Social: Living alone post-breakup. Graphic designer. ↓ Social interactions, ↑ alcohol, no drugs.
Family: Mother: MDD. Uncle: Bipolar. No suicide/psychosis history.
Goals: Regain normalcy, ↑ sleep quality, coping strategies.
After entering your notes, click "Start Template and Generate Data"
Note: DAPNotes doesn't require any Protected Health Identifying information to generate a template for DAP documentation. So do not enter any such PHI information.